Saturday, May 30, 2009
Friday, May 29, 2009
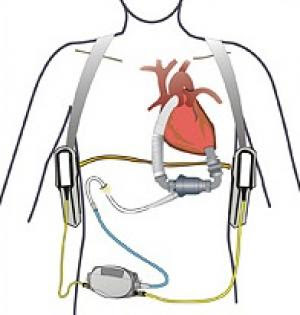
What is an LVAD?
An LVAD, a Left Ventricular Assist
Device, also known as the artificial heart, is attached to the patient's
heart for the purpose of pumping blood through their body. The
patient's heart is in a condition that can no longer pump blood itself.
There are strick requirements to qualify for an LVAD. One is that the
patient must first qualify for a heart transplant. Another is the
patient must be in severe end-stage heart failure.
This page is not intended to be
used for detailed technical information. I would like to clarify that I
am writing this casually from my experience. If you require technical
information, please go to Thoratec.
As shown below, the LVAD
connects to the base of the left side of the heart and also to the
aortic valve. The blood is detoured this way and then circulated through
the body. The pump is very quiet. Is it continuous flow, not a pump at
all really. I hardly have a pulse and a blood pressure. It's difficult
to read vitals on me. An EKG is very disturbed and doesn't look like an
EKG at all. But somehow, the doctors know what to look for and monitor
me very carefully.
The percutaneous
lead, also known as the drive line, is connect at one end to the LVAD
inside of me, exits my skin and connects to the controller. The
controller is the brain of the pump, if you will. It records my numbers,
such as speed, flow, etc. and alerts me if anything occurs that I
should be aware of. Such a case would be when the batteries are low,
when the drive line is disconnected, when the controller is not
functioning properly or the pump stops. The power source connects to the
controller. I can have three different sources of power. One,
batteries; two, the Power Base Unit (PBU); and three, the back-up
battery. The batteries are mobil so I am on them all day. They actually
last the whole day for me, about 15 hours. I'm connected to the the PBU
at night because the alarms are much louder and would wake me up if
something was to go wrong. It is plugged into the wall and has a monitor
with my numbers. The back-up battery is an additional power source in
case of an emergency. This could occur if the power went out, I didn't
have any charged batteries AND I couldn't drive anywhere to get power
from a generator elsewhere. I would like to think this would never
happen but I have it just in case.
How do I carry everything, you ask?
Well,
I have bags from practical to stylish! My most popular, and by far most
practical, is my MEC backpack. It's actually a water pack for athletes
so it's very sleek and light. I can be hands free and I often forget I
have it on. It has nice support, which is a benefit because I where it
just about all the time. I can fit all of my equipment into a couple of
stylish purses, as well. You would never know that I'm supported by such
an important, life-saving device. Some people choose to wear the
holsters and others choose to wear a fanny pack. It is a personal
decision.
Since
anything could potentially go wrong at any time, I am required to carry
my spare parts at all times. I have a few means of doing this as well.
When Shaun was with me for the first few months he would carry my parts
in his back pack. It made me feel better because I wasn't the only one.
Now, since I am getting out without him I have a small suitcase on
wheels. In this bag I must carry spare batteries, a spare controller, a
spare clip, a spare alarm battery, dressing materials (in case I spill
on the drive line exit site) and emergency contact numbers. If I want to
get out for a walk I use my school backpack and put my connected parts
as well as my spare parts in the one bag. This makes for additional
exercise!
My doctor
was kind enough to send me a copy of my xray. I found it incredibly
interesting so I thought I would share it. There is a cloudy part that
everything is connected to, that's my heart. You can see the details of
the LVAD, my ICD (Ivan) and the wires along my sternum. There is ALOT
going on in there. Metal detectors would scream at me!
There are
some limitations I must remember while supported by the LVAD. I must
avoid any significant static shock, ie. vacuuming rugs, touching tv
screens. I cannot swim or be immersed in any water. I have a shower bag
that is particularly designed for the LVAD. I cannot jump since the
LVAD could disconnect from my heart. I cannot be in a car seat that has
airbags. If they were to fire it could also disconnect the pump. I
cannot have an MRI, which was also considered when I had Ivan implanted.
The settings of Ivan cannot be changed because it interferes with the
LVAD. I cannot sleep or lie on my stomach because of the drive line exit
site. It seems like a lot but really I just get used to not doing
particular things and forget about it.
What does it feel like inside you?
Another
good question. At first, it hurt like words I cannot type here. I am
smaller than the average patient and the LVAD barely fit in. For a good
three months or so I was in constant pain. It would rub against my ribs
and I would feel it's weight shift whenever I moved. Other pain would be
associated with having open-heart surgery. For a while now, I have been
off all pain killers and I really don't feel any pain. I honestly
forget about the device and just go on living. That's the goal, right? I
am very sensitive to anybody going near my abdomin, though. As you can
see from the xray, there is reason to protect it.
I feel the
humming if I put my hand over the LVAD and I can hear the humming when I
don't have a shirt on. I often don't notice. I think I'm merely
desensitized to the device. It's just the way it is.
How do you handle it emotionally?
To keep it
simple, I really try not to think about the difficult things and take
advantage of living. I feel great and I want to enjoy it. I am
battery-powered. And I am proud to be given a second chance at living. I
want to make the most out of this opportunity. If I go tomorrow, I
don't want to be remembered for the things I complain about, I want to
be remembered for the difference I made.
It does suck, don't get me
wrong. But there is nothing I can do to the change it. I only have the
power to change what's next. And so I embrace all that I can, tell those
close to me that I love them, and just keep going. What would you do?
Thursday, May 28, 2009
About Andrea
Well I have experienced quite a
journey to stay true to my heart. It's been a long road but I feel I
have found the right direction and along with it, where I can make a
mark on this world.
It all began in May of 2008 when I was diagnosed with idiopathic dilated cardiomyopathy.
At first I didn't understand the severity of this disease and expected
that I would take meds, get better and continue on the path we had
planned. Through an experience of heart failure and the implantation of
an ICD, Implantable Cardioverter Defibrillator, we began to understand that things will need to change.
I had been with Shaun for about 4
years prior to diagnosis. We bought a house together, adopted some
pets, and discussed our future. Three weeks after I was diagnosed with
heart disease, he proposed to me. The future in general became unclear,
but we knew one thing for sure, however long we had, we wanted to spend
that time together. He is my rock, my knight in shining armour. He has
made this disease easier to cope with and given me something to fight
for. At the time, I didn't understand what that really meant and how
true it would become.
So I was told that I would just
have to live with 20% left-sided heart function. I was not severe enough
to be added to the transplant list, although I was being followed be an
out-patient clinic. I had my ICD, affectionately named Ivan, and that
was the most important thing to prevent against sudden death, a
blunt comfort.
When 2009 began I planned my
wedding. I planned it all. It was so much fun. I wasn't in a condition
to work, as of yet, so I made this my job. I made my flowers, the cake,
the favours, the invitations, the thank-you cards, and organized
everything. We married in May of 2009 and the day was absolutely
beautiful. I married the man of my dreams. Committed my life to him in
front of all my dearest family and friends. As the night passed on, we
had dinner and began our speeches. Shaun and I decided to do our speech
first so we could relax for the others. Well Ivan was not happy with the
speech and decided to make his presence known. Two minutes into the
speech he fired three times. My new husband caught me before I fell to
the floor. I was taken to St. Mary's Hopsital in Kitchener, not knowing
that this hospital would later save my life.
The nurses and staff planned a
little party for us and our family in the hospital that night. We were
able to cut the cake, throw the bouquet and have a toast. They treated
me wonderfully and made the difficult experience a little better.
The summer of 2009 brought some
strange symptoms. Through about 3 months of abdominal pain and
difficulty eating it was determined that I was in SEVERE heart failure.
It was a nurse at St. Mary's that got me to see a doctor. My existing
cardiologist continuously told me it was a gastrointestinal issue, as
did ER doctors and surgeons. None-the-less, I got to the right people.
They treated me and determined my condition was more severe than their
facility could handle and they sent me to Toronto General Hospital to be
evaluated for transplant.
I was then approved on the
transplant list and experienced the fight of my life. Hooked up to about
15 IV's did nothing to improve my condition. I waited three days for a
heart to become available but I was not able to wait another day. The
doctors implanted the LVAD, a Left Ventricular Assist Device
to pump blood through my body since my heart was not able to do it
alone. This was life saving surgery and I feel it is my second chance at
life. It's purpose is a "bridge to transplant". I am still waiting for a
heart transplant.
I would like to make a change in
this world. I will share my experiences to promote organ and tissue
donation and blood donation. Everyone wants to know what they can do to
help, make a change, inform yourself and become an organ and tissue
donor.
Subscribe to:
Comments (Atom)